BBC Three
BBC ThreeThe truth about early menopause
Hot flushes, mood swings and dryness downstairs - three women tell us what it's like to face the end of their fertility before reaching 30
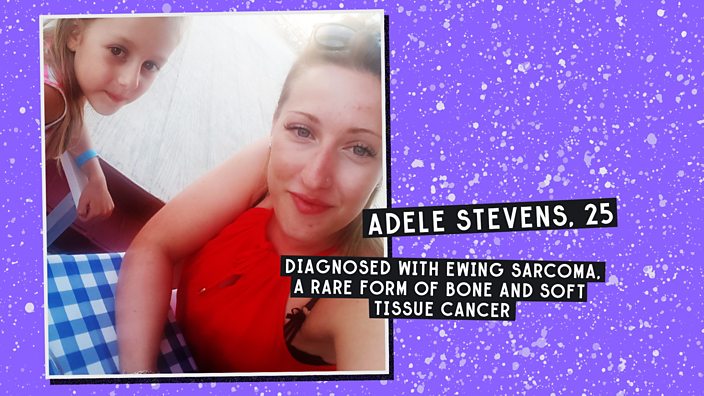
Most women don't even think about the hormonal roller coaster that is the menopause until they hit their mid-40s, with 51 being the average age for women's periods to actually stop. But Adele Stevens is dealing with hot flushes, mood swings and the end of her fertility aged just 25. To make matters worse, she’s going through it at the same time as her mum, who is in her 50s.
Adele is a mum herself, to a six-year-old daughter. "All my friends are having babies at the moment and I still want another one, but I don’t know if it’s possible now," she says.
This is happening to Adele because four years ago she was diagnosed with a rare form of bone and soft tissue cancer, Ewing sarcoma.
"A lot of things went through my mind when I first got my cancer diagnosis, but the menopause wasn't one of them," she says. "I didn't even know that chemotherapy could affect your fertility until my mum asked my doctor about it."
Fertility problems are probably one of the lesser-known side effects of many cancer treatments. As if the C word isn't a big enough bombshell to come to terms with, many young cancer patients like Adele also have to grapple with the possibility that they might not be able to have kids afterwards.
"When the doctors first told me my treatment would probably make me infertile, I was stunned,” says Adele. “I didn't know what to say, just 'Oh, wow, okay'. It all happened so fast there wasn't even time to freeze my eggs," she recalls.
But not all cases of early menopause are the result of cancer treatment. Sometimes known as Premature Ovarian Failure (POF), or Primary Ovarian Insufficiency (POI), early menopause affects roughly one in every 100 women under 40, one in every 1,000 women under 30, and one in 10,000 under the age of 20, according to support charity The Daisy Network.
 BBC Three
BBC ThreeIn 90% of cases it is spontaneous and idiopathic, which means the cause is unknown and doctors can't find a way to explain it.
"As the name suggests, premature ovarian failure is where the ovaries run out of hormones earlier than expected, before the age of 40," explains Professor Ying Cheong, an expert in reproductive medicine at the University of Southampton.
"It’s where younger women suffer the symptoms of menopause – irregular periods, hot flushes, night sweats, vaginal dryness, cognitive difficulties like memory loss, and decreased sexual function and desire," she adds.
This is what happened to 24-year-old Annabel Oakley-Watson. She was just 15 and had only ever had one natural period, when she was diagnosed with early menopause.
"I had one period when I was 13 and then they just stopped. After several blood tests and six months of trying different contraceptive pills to regulate my hormone levels, I was told I'd already experienced my menopause and there was nothing that could be done," she says.
The thought she might never be able to get pregnant and have a family was a huge thing for Annabel to take in while she was still in her teens.
"After my diagnosis it hit me really hard that I'd never have a baby of my own. I would watch One Born Every Minute and cry the whole time," she says.
"I've always thought giving birth must be such a special moment for a couple," she adds. "I was angry that the chance to experience it had been taken away from me.
"When I went to university at 18, I was prescribed hormone replacement therapy (HRT) to manage the menopause symptoms but I was so angry and in denial, I just didn't take it," Annabel recalls.
"I just wanted to feel normal. At university I was living with a group of girls, which was great, but a lot of our chat was about periods and sex and boys."
 BBC THREE / OLIVIA BOHAC
BBC THREE / OLIVIA BOHACLooking back, Annabel says she can see that not taking her HRT pills made her symptoms worse. "I was pretty nasty to people because of the mood swings. I felt tired, lethargic and angry."
"I feel happy and grounded on HRT now. I was just so young then," she adds. “I was jealous of my friends – I'd order free samples of tampons online, just hoping that something would change. It took me a long time for me to accept that it wasn’t going to."
Although early menopause can't be medically explained in the majority of cases, it can sometimes be induced by other treatments – including certain cancer treatments and surgery to remove the ovaries.
This is what happened to 23-year-old Katy Johnston. She suffers from severe endometriosis – a painful condition where the tissue which lines the uterus grows outside the womb. She has been on a course of hormone injections for the last nine months, which have caused her to experience temporary menopause.
"In effect, they press pause on ovulation – so, in theory, they should reduce the spread of my endometriosis, a condition which worsens every time I have a period," she explains. "The process is temporary, while I wait for further surgery but sometimes it feel like I've aged 30 years in the space of a few months."
In Katy’s case, the menopause is both a blessing and a curse. "The symptoms aren't great. They're hot, but not in the sexy sense!" she says. "I have hot flushes, which are worse through the night; I'm hairier and more forgetful and my concentration is shot. I still get some breakthrough bleeding and cramping pains and sometimes I feel like I'm getting the worst of PMS and the menopause all at once."
Despite all that, she says, her quality of life has significantly improved. "When I started this treatment, I’d been basically housebound for about two months. Before that, there'd be three days every month when I couldn't leave my bedroom because my periods were so painful," she says.
"At first, I worried that it might somehow not be temporary – like, will my ovaries definitely 'turn back on'? But I've learned to relax about it," she says. ”Honestly, I'd take hot flushes over agonising cramps any day.
"Now, I'm able to go to work and uni – live the life that had been on pause up till this point. It's been a total game-changer and I'm so grateful, but it's not a long-term solution," she adds. "Prolonged use of these drugs could have devastating side effects like osteoporosis, which weakens your bones, that scares me."
 BBC Three
BBC ThreeAll these women have been forced to confront their fertility and worry about its decline, at a far younger age than their peers.
Adele and her partner made it clear to doctors they wanted to have another child, so a new cutting-edge treatment called ovarian cryopreservation, which may help to restore her fertility further down the line, was suggested.
"Basically, before I started chemotherapy, they removed my ovary, sliced it up, and then froze all the different slices. Then they can re-implant it later, and hopefully it should start to grow back as healthy tissue," Adele explains. "I was told there's only about a 30% success rate but I wanted to try anything I could."
"I didn't have a period throughout the 10 months I was in treatment, or for about 10 months afterwards,” Adele explains. “Then I started having irregular periods, getting really hot, and having night sweats and mood swings. It's put a strain on my relationship with my partner because he can never tell how I'll be from one minute to the next."
But by far the biggest challenge for their relationship, Adele adds, has been the uncertainty around her future fertility. "The symptoms I can deal with, I just have to ride it out. But my partner and I are desperate to have another child together and I don't know if I'll be able to give him that," she says.
If her ovaries are successfully re-implanted, the healthy tissue should reverse Adele's menopause and allow her to try to conceive naturally. For Professor Cheong, it's a really exciting new development. "It's still deemed experimental but, in my opinion, it won't be long before it becomes mainstream. It really opens up new opportunities for people to preserve their fertility in situations like Adele’s," she says.
Adele's operation is now booked for 17 December. Going through this process, she says, has made her feel more positive about the future.
"Whatever happens, I always try to remind myself that beyond fear lies freedom,” she says. “Despite everything I've been through - cancer, the menopause - I'm still only 25 and have my whole life ahead of me. I'm determined to make the best of that for me and my little girl."
To find out more watch The Menopause on BBC One on 26 November at 21:00 GMT
This article was originally published on 29 November 2018.