- 1Department of Public Health, University of Otago Wellington, Wellington, New Zealand
- 2Māori/Indigenous Health Institute (MIHI), University of Otago Christchurch, Christchurch, New Zealand
- 3Department of Psychological Medicine, University of Otago Wellington, Wellington, New Zealand
Introduction: Clinician bias contributes to lower quality healthcare and poorer health outcomes in people with mental health and substance use conditions (MHSUC). Discrimination can lead to physical conditions being overlooked (diagnostic overshadowing) or substandard treatment being offered to people with MHSUC. This research aimed to utilise experiences of people with MHSUC to identify discrimination by clinicians, including the role of clinician’s beliefs and assumptions in physical health service provision.
Methods: We surveyed people with MHSUC who accessed physical healthcare services. Of 354 eligible participants, 253 responded to open-ended questions about experiences of those services. Thematic descriptive analysis of survey responses was completed using existing stigma frameworks and inductive coding.
Results: One dominant theme from survey responses was that diagnostic overshadowing by clinicians was driven by clinician mistrust. Another theme was that clinicians assumed respondent’s physical symptoms, including pain, were caused by MHSUC. This influenced decisions not to initiate investigations or treatment. Respondents perceived that clinicians focused on mental health over physical health, contributing to suboptimal care.
Discussion: Discrimination based on MHSUC leads to poor quality care. Health systems and clinicians need to focus quality improvement processes on access to and delivery of equitable physical healthcare to people with MHSUC, address stereotypes about people with MHSUC and improve integration of mental and physical healthcare.
1. Introduction
People with mental health and substance use conditions (MHSUC) experience worse outcomes from physical health conditions than those without MHSUC (1–4). This can be attributed in part to poorer quality physical healthcare, including lower rates of timely, appropriate diagnosis and treatment (5, 6).
People with MHSUC presenting to a health service with a physical complaint commonly experience the complaint being dismissed or ignored (7–10). When physical symptoms are misattributed to MHSUC, with subsequent missed or incorrect diagnoses, this is described as diagnostic overshadowing (11, 12).
Even when physical conditions are recognized, differential outcomes may still occur if clinicians provide different treatments or fail to address barriers to care for people with MHSUC (11). Therapeutic pessimism or overshadowing can contribute to clinicians developing inferior treatment plans for people with MHSUC, driven by negative beliefs about a person’s capacity and ability to comply or respond to treatment (11, 13).
Bias from clinicians plays an important role in both diagnostic and therapeutic overshadowing (11, 14, 15). Bias encompasses a range of factors, from lack of experience or knowledge about mental health (ignorance), negative beliefs about people with MHSUC (stereotypes), negative attitudes and emotions towards people with MHSUC (prejudice) and discriminatory behavior (discrimination) (16, 17). Bias can also be unconscious or implicit, and bias against people with MHSUC occurs in clinicians at similar high levels to the general population (18, 19).
Previous research in Aotearoa New Zealand (NZ) reported that 23% of people with MHSUC experienced discrimination from health services (20). Examples of discrimination include acting on stereotypes and prejudice, such as clinicians avoiding patients with MHSUC due to unwarranted fear of violence or discomfort with mental illness (21) and patients with MHSUC being denied weight loss surgery due to unsubstantiated assumptions they will have poorer outcomes (22). Discrimination from clinicians can also deter people from seeking treatment (23), creating further barriers to appropriate diagnosis and treatment of physical conditions.
Although qualitative research has examined reasons for overshadowing from the perspective of clinicians (10, 21, 24), exploring discrimination from the perspective of people with MHSUC is less common and usually limited to describing discriminatory behavior without identifying underlying stereotypes (25–28). We surveyed people with MHSUC in NZ who had accessed healthcare for a physical health condition, drawing on methodology that also used patient perspectives to critique service quality issues (29, 30).
The aims of the research were:
• To describe how people with MHSUC experienced discrimination in physical health services, including diagnostic and therapeutic overshadowing.
• To use the observations and reports of people with MHSUC to explore likely underlying beliefs of clinicians that lead to discrimination in physical healthcare.
2. Materials and methods
Experiences of physical healthcare in people with MHSUC were collected through an anonymous online Qualtrics survey that included both closed and open-ended questions and ran from 31 January to 1 April 2022.
2.1. Recruitment and sample
People were recruited through snowballing methods using digital media, starting with social media outreach through Facebook and Twitter by the researcher team and research advisory group and distribution through online newsletters and email lists from other organizations (e.g., Government and non-governmental organizations and services, Māori health networks and providers).
The survey site was accessed 488 times. Four-hundred-and-eight people agreed to participate, and 354 eligible individuals were included in the final dataset. Eligibility criteria were:
• Use of primary or secondary healthcare services for MHSUC in the past 5 years
• Engagement with any health care service for a physical health issue in the past 5 years
• Age 18 or over.
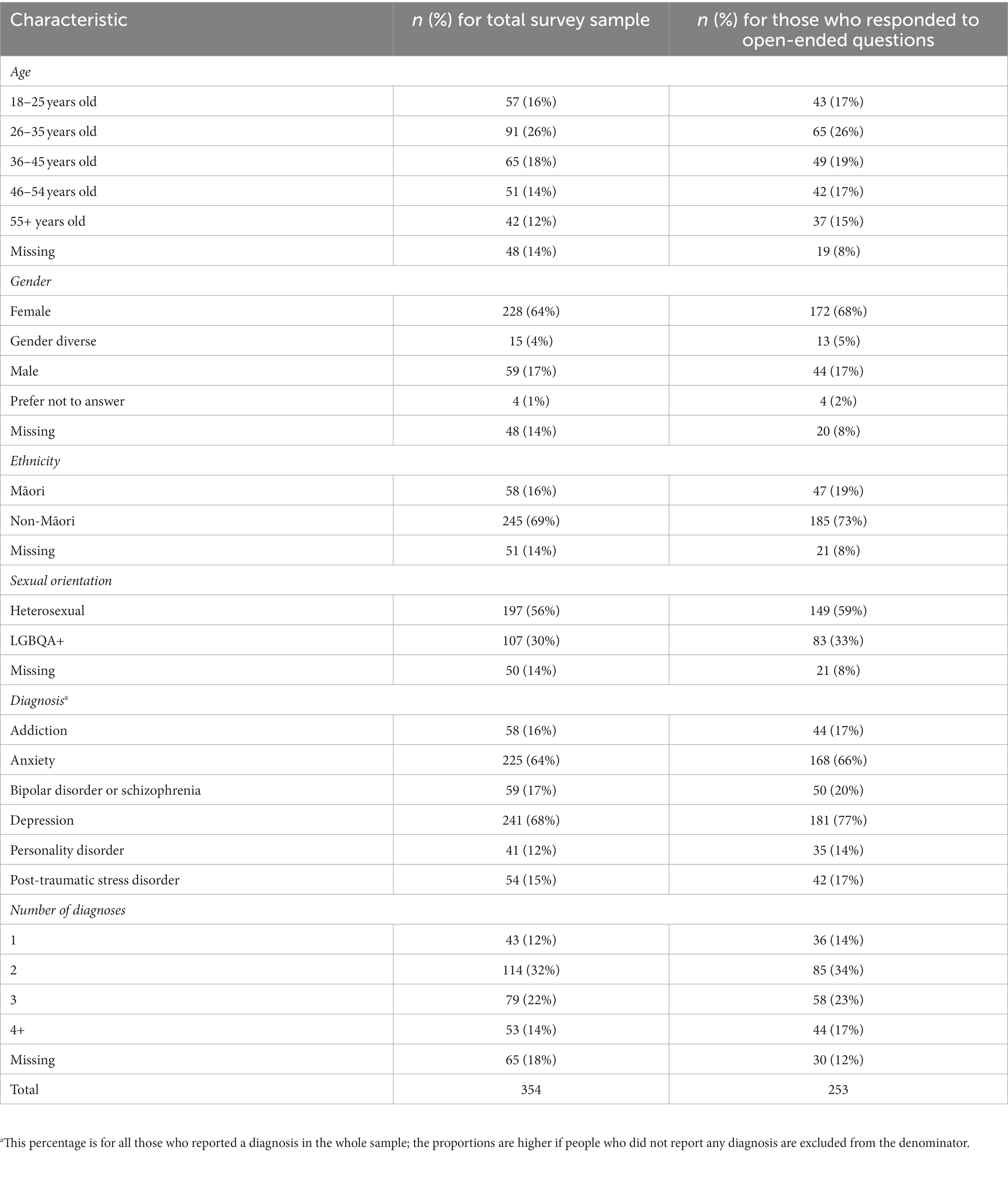
People who did not answer any questions about physical healthcare services were excluded, as was one duplicate response. The analysis sample for this paper included only those who answered at least one of the open-ended questions (n = 253).
2.2. Survey content
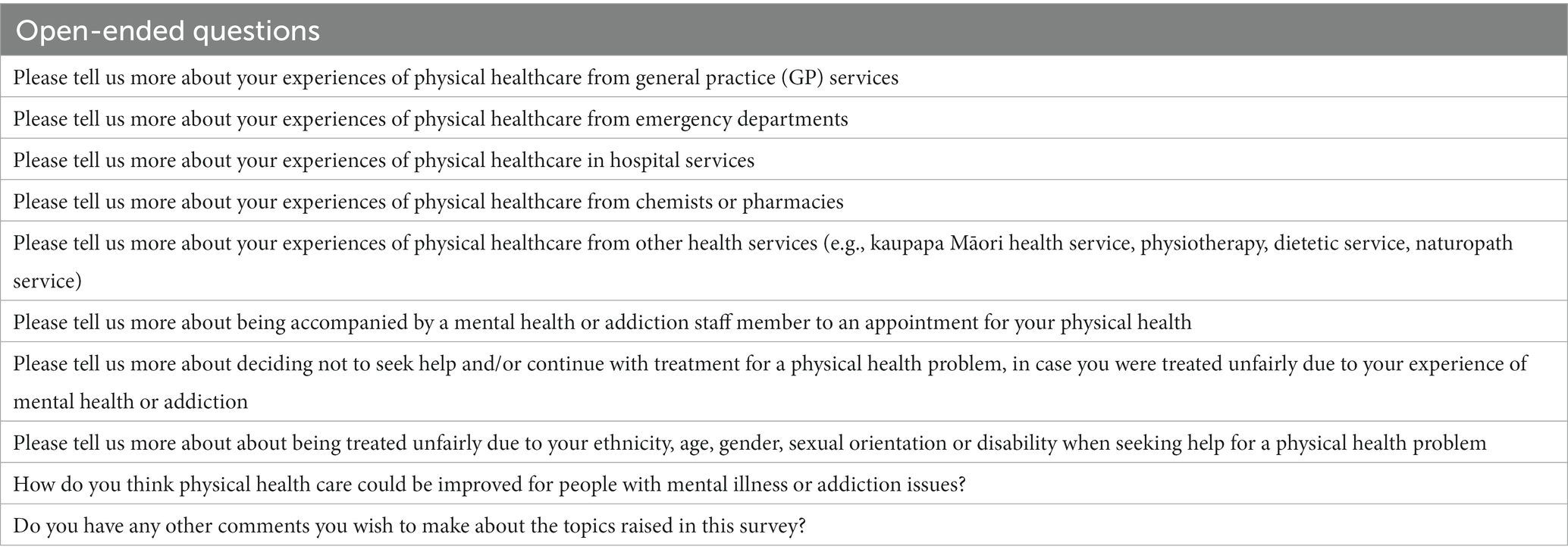
The survey was divided into four sections covering mental health and addiction service use, physical health service use (across five types of services), stigma and discrimination, and demographics. Demographic questions included age, gender, ethnicity, sexual orientation, and MHSUC diagnoses. The survey questionnaire was reviewed by a research advisory group, which included clinicians and people with lived experience of MHSUC. The responses to ten open-ended questions formed the basis of the qualitative analysis (Table 1).
Ethics approval was granted by the Southern Health and Disability Ethics Committee (21/STH/216). Information about the survey, including maintenance of privacy and confidentiality, and contact details for support was provided in the survey introduction. Informed consent was assumed once participants engaged with the online survey. Where identifying information was provided by participants (in order to volunteer for participation in interviews or to receive study results) this information was removed prior to analysis and stored separately and was not accessible to study authors conducting analyzes.
2.3. Data analysis
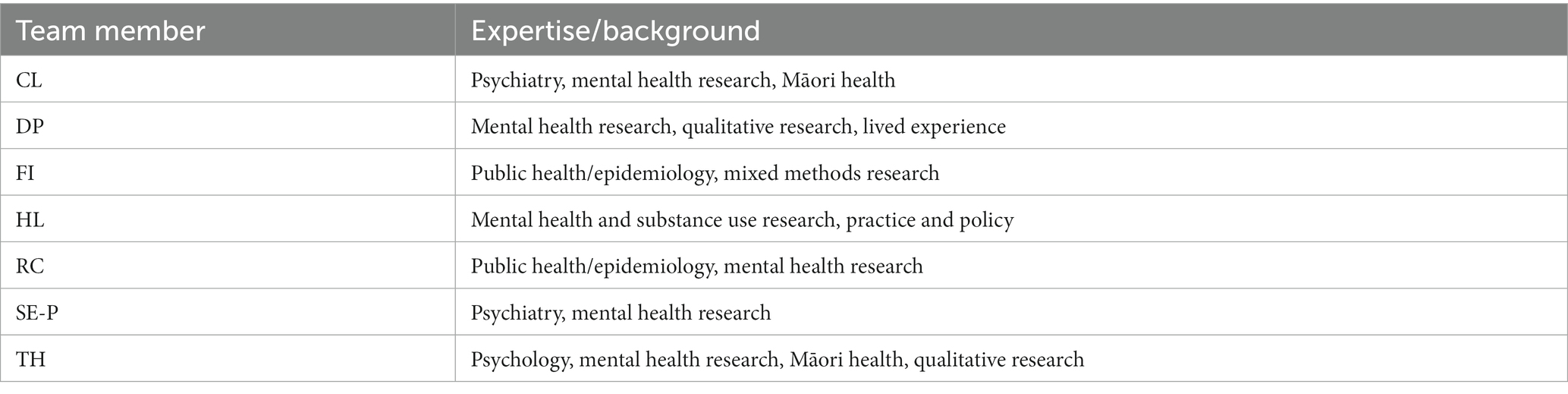
Responses to the open-ended questions were imported into NVivo v1.6.1 (QSR International) in an anonymised form. We used theory-driven thematic analysis (31), starting with deductive coding using pre-existing frameworks on stigma (16, 17) to classify experiences of discrimination. Investigators (FI and DP) independently reviewed survey responses to identify sections of text that described discrimination, prejudice and stereotypes. These sections were analyzed inductively to infer clinicians’ underlying assumptions as perceived and reported by respondents, drawing on the respondents’ observations of clinician demeanor and behavior and their interpretations of these, particularly within the context of delayed, missed or incorrect physical health diagnoses, but also where physical health diagnoses were unknown or unclear. The investigators discussed and developed themes based on respondents’ common experiences as an iterative process with team input and review (Table 2). Quotes to demonstrate themes were inserted verbatim with grammatical corrections to aid clarity and identifiers indicating age range (NA = no age given) and gender (W = woman, M = man).
3. Results
3.1. Respondent characteristics
Respondents were predominantly female and compared to the general population were younger and more likely to identify with the rainbow community (Table 3). Depression and anxiety were the most frequently reported MHSUC diagnoses and multiple diagnoses were common.
3.2. Overview of themes
Three themes (clinician’s beliefs) were evident from the descriptive analysis of factors that people with MHSUC considered led to discrimination from clinicians when seeking physical healthcare. Themes included that in people with MHSUC, MHSUC is responsible for physical symptoms (with sub-themes around physical symptoms being psychosomatic, caused by anxiety and pain as an unreal symptom), that people with MHSUC are untrustworthy (particularly those who need controlled drugs or pain management) and that mental and physical healthcare were competing priorities (either mental or physical health takes the focus).
3.3. In people with MHSUC, MHSUC is responsible for physical symptoms
A predominant theme from survey respondents centered around the experience of clinicians assuming that their MHSUC was responsible for or explained their physical symptoms. As a result, respondents reported that their physical symptoms were dismissed, leading to delayed investigations, diagnosis and treatment – or no investigation despite an underlying physical cause. Respondents reported that they were not treated in the same way as someone without a history of MHSUC.
I had to argue with a doctor about the cause of dehydration and difficulty swallowing. He put it down to depression and a history of eating disorders. Turned out I had thrush in my mouth and oesophagus after being on antibiotics. (W, 36–45)
Within this theme, sub-themes emerged relating to physical symptoms in people with MHSUC being ascribed as psychosomatic, or due to anxiety and stress, and the physical symptom of pain being not real or caused by MHSUC.
3.3.1. Physical symptoms in people with MHSUC are psychosomatic
Respondents reported that clinicians assumed their physical health symptoms were either psychosomatic or not real. Whether clinicians distinguished between psychosomatic conditions and “feigning” was unclear, but respondents were left with the impression that their symptoms were imagined.
I was in for cardiac issues. When ECGs were done because of chest pain and came back normal it was suggested it could be because of my bipolar by nurses again. It was in fact my Duromine that I was on for weight loss, so it wasn’t in my head at all. (W, 55+)
Although respondents frequently experienced clinicians telling them that physical complaints were psychosomatic or due to their MHSUC, they were not told what this meant or what to do about the symptoms they were experiencing, leaving them unclear how to manage and reluctant to raise the same or other concerns in the future. Respondents experienced this as a bind, where the onus was on them to prove their symptoms were not caused by their MHSUC, and if they could not, they were left without treatment or support.
In some instances, my mental health issues are blamed for my physical health issues but it is never explained why my [mental health] is to blame. I leave feeling hopeless and confused.(W, 26-35)
3.3.2. Physical symptoms in people with MHSUC are due to anxiety and stress
Respondents reported that anxiety and stress were the primary reasons given by clinicians to explain physical symptoms, and the reasons for not investigating further. Examples of this spanned both primary and secondary healthcare settings. Several respondents who were initially told that their physical symptoms were due to anxiety or stress were later diagnosed with significant health conditions, including lupus, a kidney infection, a viral liver infection, endometriosis, brachial neuritis and postural tachycardia syndrome.
My GP often tries to blame any physical problem I have on my anxiety. I know my own anxiety pretty well now, I know what it feels like and how it behaves. It frustrates me when my GP is not willing to investigate my symptoms and just says “it could be your anxiety.” (W, 26–35)
3.3.3. The physical symptom of pain in people with MHSUC is not real or is caused by MHSUC
A special category within this theme related to pain as a physical symptom. People with MHSUC complaining of pain experienced an even stronger sense that their clinicians believed the pain to be imaginary or fabricated and did not warrant treatment. People were given the impression that their MHSUC caused or exacerbated pain, or they could not achieve pain control unless their MHSUC was better managed.
In the last 5 years I have been struggling to get a diagnosis and get treatment for on-going pelvic and back pain as a result of adenomyosis, a pars defect and a few other factors. My mental health would be brought up in every appointment and often blamed for my inability to control my pain levels. [This was] despite already seeing a psychologist and psychiatrist, being on medication, and being in decent control of my mental health. (W, 26–35)
Poor treatment of the symptom of pain could relate to mistrust of people with MHSUC (and reluctance to prescribe pain medication, see below) and/or lack of knowledge about the nature and management of pain. One respondent reported her experience: “I was told that I could not possibly be in pain as my car accident was years ago. The woman told me to repeat after her, ‘tissue damage repairs itself after 3 months so I am not in pain.’” (W, 46–54) That this occurred at a pain clinic suggests that ignorance was not the root cause of this dismissal, as such clinics routinely assess people with pain that persists in the absence of tissue damage.
3.4. People with MHSUC are untrustworthy
Respondents recounted how they were not believed when they reported physical health symptoms, with an implicit or sometimes explicit assumption that they were making the symptoms up, exaggerating or even outright lying. The presence of an MHSUC diagnosis was presumed to indicate an unreliable narrator.
I broke my tailbone and sacrum I was called a liar, I'm faking it, etc etc. Turns out was so serious, my insides were prolapsed, tailbone removed, sacrum has 3 pins in but took me 2 years, lots of tears … hundreds of pain meds for them to believe me. (W, 46–54)
Respondents felt ignored, dismissed and not listened to. Respondents wanted their physical health concerns to be taken seriously, independently from their MHSUC diagnosis, and without fear of their symptoms being pre-determined as having a psychological aetiology.
Doctors have been quite dismissive, I've felt, of the physical symptoms I’m experiencing, almost always putting it down to my mental health challenges which at times is frustrating. I just wish they would listen a bit more and not immediately discount physical health complaints because I have a mental health diagnosis. (W, NA)
The experience of being disbelieved and dismissed could have negative consequences for people’s mental health, making it even harder to seek help for physical health issues.
I find seeing a new doctor a very stressful experience now, especially if they already have my patient notes, because I have to prepare to not be listened to, talked down to, or entirely dismissed. (W, 26–35)
3.4.1. People with MHSUC who need controlled drugs or pain management are particularly untrustworthy
Within this theme, the experience of being untrustworthy was intensified for people with addiction or taking controlled medication. Mistrust was most evident in relation to pain management and pain medication, and particularly affected people with addiction or perceived to be at risk of addiction, who could be labeled as drug seeking. They found it difficult to access pain relief and even routine investigation or treatment for symptoms.
Referred to mental health labeled as an attention/drug seeker. I had heart failure. (W, 55+)
The experience of mistrust extended beyond people with a history of addiction. People with mental health conditions but no history of addiction still felt they risked being labeled as a ‘drug seeker’ if they presented with pain. The consequence of this mistrust was that some people did not receive pain relief and others did not even ask for it, due to lack of confidence and a mutual lack of trust in clinicians and the health system.
I’m on a controlled drug for ADHD and feel that often I am treated as a criminal and a drug seeker both by my GP service and my regular pharmacy. Makes me loath to disclose any issue with pain or my anxiety as I know they will judge it as drug seeking behavior. (W, 36–45)
3.5. Mental and physical healthcare are competing priorities
People with MHSUC experienced two apparently conflicting assumptions related to the intersection between mental and physical healthcare, depending on the context and the focus of the clinician, which could be at odds with what the patient wanted to focus on.
3.5.1. Mental healthcare takes the focus over physical health
The first assumption was that mental health issues must be attended to first before any physical health concerns could be addressed. The MHSUC was the primary or sole focus, even when people presented only with physical health concerns. Sometimes this was to the extent that clinicians appeared to be unable to deal with physical health conditions when there was co-existing MHSUC.
I went to seek help for a sore ankle, the Dr replied with a “tell me about your bipolar disorder.” Turns out I had a torn ligament, diagnosed by someone else. My treatment was delayed and I felt humiliated. (W, 36–45)
Respondents wanted to be seen as people, not as “mental health cases.” They wanted their physical symptoms to be treated as important and to be addressed fully and actively. They wanted physical causes to be ruled out first, rather than the MHSUC to dominate the consultation.
My mental health becomes a significant distraction and delays getting actual treatment for the issue I was there for. I wanted to know about my baby, but the conversation always went back to my mental health. I was stressed because I wanted to enjoy and understand my pregnancy, but no-one talked to me about my baby. I thought that’s what I was there for. (W, 36–45)
3.5.2. Physical healthcare takes the focus over mental health
The second assumption pertaining to the relationship between physical and mental healthcare was that a person’s MHSUC had no impact on their physical health and that mental health concerns could be left to some other clinician or service. This appears to contradict the assumption that mental health takes the focus but demonstrates how mutually exclusive beliefs can exist within the same system.
Most descriptions of this assumption related to physical health services not understanding or accounting for stress and anxiety related to procedures, treatment or health settings or MHSUC being overlooked when it was relevant to physical healthcare.
I have Type 1 diabetes and am an outpatient at the diabetes clinic. Mental health is not addressed as a component of diabetes care, but in my experience, there is a lot of connection between my diabetes management and mental health. (M, 36–45)
Some of the tension between whether mental health or physical health was prioritized related to a lack of clarity over who was responsible for each domain of health. Holistic care, where physical and health issues were both treated as important and the interdependencies between them were recognized, was an ideal that respondents felt was rarely achieved.
The focus with some services is only on one thing – they do not take a holistic approach to wellbeing. If I am there for a physical issue then my mental health is not discussed and vice versa. (W, 26–35)
Short appointment times in primary care meant that some respondents felt that mental, addiction and physical health concerns could not both be adequately addressed in a single consult – this may have been dependent on service attributes of the practice and clinician. Although mental health was often assumed to be the cause of physical symptoms, the impact of physical health on mental health was seldom raised by clinicians.
4. Discussion
Respondents in this study provided many examples of how the demeanor and responses of clinicians would change or differ depending on their awareness of the respondent’s MHSUC, and the ways in which their MHSUC led to diagnostic and treatment overshadowing, contributing to delayed treatment and prolonged suffering.
Although research into the prevalence and impact of overshadowing is lacking (32), previous studies have documented adverse outcomes from diagnostic and treatment overshadowing (7, 10, 12). For example, in a qualitative study of clinicians working in the ED, clinicians recalled two patients with MHSUC who died and five who experienced irreversible long term damage due to delayed investigation or treatment (10). From the clinicians’ perspective, factors that contributed to overshadowing included difficulties in taking a detailed history, frequent attendances for unexplained symptoms and patients refusing to consent to an examination, procedure or treatment (10, 21). Poor interpersonal skills and lack of collaborative care from health providers were additional contributing factors (7, 21).
These studies convey how features of the patient and how they present contribute to overshadowing, explicitly or implicitly focusing the blame on the person. Treating patients differently because of any characteristic is discriminatory behavior, whether due to an individual clinician’s prejudice (33) or a system failure to accommodate the needs of patients (25, 28, 32, 34). By taking the perspective of the patient, we sought to focus on the clinicians’ actions, in order to shift responsibility onto services and systems to provide non-discriminatory care.
4.1. Addressing the psychosomatic assumption
Many respondents in this study reported that physical symptoms were attributed to their MHSUC almost by default, with no apparent consideration of a somatic cause. Without access to patient notes and records, we were unable to verify whether any or some appropriate investigations or examinations were conducted, but in many cases, the stories spoke for themselves – physical health conditions, including broken bones and infections, were missed.
This indicates not only discrimination but a failure in the duty of care, as presenting symptom(s) in all patients should be thoroughly investigated, regardless of previous history, which may include interviewing family or other contacts to gather additional information (10).
The assumption that MHSUC can cause physical symptoms may be true, as medically unexplained symptoms are extremely common, particularly in primary care (35). However, even in these situations, this does not mean that symptoms are not real and does not excuse a clinican from investigating for an organic cause and offering treatment or a referral if this is outside their expertise (36, 37). In the face of unexplained symptoms, clinicians are encouraged to reflect on the number of medical conditions throughout history that have been considered “psychosomatic” but subsequently found to have a biological basis (38).
4.2. Addressing stereotypes
Addressing the stereotype that people with MHSUC are untrustworthy involves more than one-off education sessions or increased awareness. From research on interventions to address unconscious bias, some strategies show promise (including exposure to counter-stereotypical examples, identifying with the outgroup and emphasizing the recovery from MHSUC) but positive effects may wane with time due to ongoing exposure to bias entrenched in society and discriminatory workplace cultures (13, 39). Interventions may need to be organization-wide and repeated, with ongoing assessment, reflection and deliberate practice (40, 41) using objective monitoring methods (e.g., internal audits against best practice standards, comparing treatment plans for people with and without MHSUC).
It is not only patients with MHSUC who are disbelieved and mistrusted. People reporting persisting symptoms after COVID infection were initially discounted, as “unreliable informants of their own illness experiences.” (42) People with MHSUC also experience discrimination in health care services due to belonging to other stigmatized groups, including female, ethnic minorities, sexual minorities and gender diverse people, which can worsen physical and mental health (43–46).
Not believing or taking a patient’s symptoms seriously is the antithesis of patient-centered care, a critical dimension of high-quality healthcare (40, 47, 48). A revised commitment to patient-centered care, with an explicit focus on respect, partnership, listening to and developing a trusted relationship with the patient, may be needed to improve quality of care for people with MHSUC.
4.3. Addressing mind–body dualism
The conflicting experiences of mental health taking precedence over physical health in some consultations and vice versa in others underscores the artificial and stigmatizing separation of mind and body within health systems (49, 50). Better integration between mental health, substance use and physical health services in order to improve outcomes for people with MHSUC is an ongoing challenge but a priority for health systems (51, 52). Characteristics of successful integration models include case management, care co-ordination and joint assessment/planning, shared information systems, co-location, clear accountabilities and strong leadership (51, 53–56). Physical health services, particularly primary care services which are often at the forefront of assessment, treatment and referral of people with MHSUC, need to have the requisite mental health and addiction training and skills (57, 58). Conversely, mental health and addiction services need to be aware of physical health risks associated with MHSUC and treatment and ensure that physical health needs are addressed (59).
4.4. Strengths and limitations
One limitation of this research was a relatively small sample size, but responses to the open-ended questions were high (71% of survey respondents gave textual answers), including some extensive narratives. However, we were unable to clarify ambiguous responses since the data were collected anonymously online. In this paper we focused on the worst experiences of physical healthcare for people with MHSUC. Respondents also recognized non-discriminatory behavior and provided exemplars of when they were treated well, which will be published separately. Responses to closed questions about quality and experience of healthcare services are published elsewhere (60). From this paper, 10% of respondents reported experiencing discrimination due to MHSUC always or most of the time, and this was significantly more prevalent in people with severe mental illness (schizophrenia or bipolar disorder), those with four or more diagnosis and LGBQA+ individuals. In addition, 20% of respondents reported diagnostic overshadowing always or most of the time, and this was experienced more often by Māori, people with severe mental illness or addiction and those with four or more diagnoses (60).
The underlying assumptions we have described are based on reports from respondents, and their interpretations of the clinician’s attitudes and behavior. We are unable to ascertain the beliefs and assumptions from the clinician’s perspective but regard the perceptions of respondents to be more valuable than clinician’s self-report in this context. Unconscious and social desirability biases are likely to lead to under-recognition and under-reporting of clinician bias against people with MHSUC. Taking the patient perspective, we are unable to disentangle whether unfair treatment is solely due to MHSUC or caused or compounded by other biases, such as racism, sexism or homophobia. More research should be done to examine the interactive impacts of belonging to more than one stigmatized group.
We were unable to quantify the impact or relative importance of assumptions that lead to discrimination against people with MHSUC. However, it is well established that people with MHSUC have worse outcomes from physical health conditions, including premature mortality (5). Further research is needed to quantify the extent of overshadowing and its causative factors and develop effective interventions to reduce it. One Australian survey found that 11% of people with MHSUC had experienced discrimination by a clinician in the previous 12 months (27).
The underlying assumptions identified in this research are consistent with findings from other studies on bias against people with MHSUC in clinicians (32), suggesting that these are not unique to NZ. However, in countries with different healthcare structures, particularly with higher levels of mental and physical healthcare integration, the competing priorities of mental and physical health may be less acute.
Respondents were self-selecting, recruited through social media and health service connections, hence may not reflect the experiences of people who are not engaged with health services or able to participate in online research. On the other hand, groups who might be more likely to experience other forms of discrimination such as women and people from the rainbow community were over-represented in our sample. However, although we would expect that more marginalized individuals would experience higher levels of discrimination, the stereotypes and underlying assumptions are likely to be similar.
5. Conclusion
Experiences of overshadowing in people with MHSUC are experiences of discrimination from individual clinicians, which may be exacerbated by personal and system factors, but are inherently healthcare quality issues. Interventions to change the way we support and manage the physical health of people with MHSUC are urgently needed.
Data availability statement
The datasets presented in this article are not readily available because due to the nature of the research, respondents of this study did not agree for their data to be shared publicly, so supporting data are not available. Requests to access the datasets should be directed to ruth.cunningham@otago.ac.nz.
Ethics statement
The studies involving humans were approved by Southern Health and Disability Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because this was an online survey. Detailed information about the survey and contact details for more information was provided at the start of the survey. Informed consent was assumed when participants chose to engage with and complete the survey.
Author contributions
RC: Conceptualization, Funding acquisition, Methodology, Project administration, Writing – review & editing. FI: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. TH: Methodology, Writing – review & editing. SE-P: Methodology, Writing – review & editing. CL: Methodology, Writing – review & editing. HL: Conceptualization, Funding acquisition, Methodology, Writing – review & editing. DP: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Health Research Council New Zealand (#20-216). The funder was not involved in the design of the study; the collection, analysis, or interpretation of data; or writing the manuscript and did not impose any restrictions regarding the publication of the manuscript.
Acknowledgments
We would like to acknowledge all the people who took the care and time to share their experiences in the online survey. We would like to thank members of the broader Tupuānuku study team, including Mau Te Rangimarie Clark, James Stanley, Sheree Gibb, and especially Abigail Freeland who was key in the development and launch of the survey. Thank you to current and past Advisory Group members who provided advice on the survey content and interpretation of results: Caro Swanson, Catherine Gerard, Ross Phillips, Tony O’Brien, Arran Culver, Sarah Gray, Suz Pitama, Suzana Baird, Vanessa Caldwell, John Robinson. This manuscript was written in accordance with the Standards for Reporting Qualitative Research guidelines.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Guidelines for the management of physical health conditions in adults with severe mental disorders. Geneva: World Health Organization (2018).
2. Walker, ER, McGee, RE, and Druss, BG. Mortality in mental disorders and global disease burden implications. JAMA Psychiatry. (2015) 72:334–41. doi: 10.1001/jamapsychiatry.2014.2502
3. Scott, KM, Lim, C, Al-Hamzawi, A, Alonso, J, Bruffaerts, R, Caldas-De-Almeida, JM, et al. Association of mental disorders with subsequent chronic physical conditions. JAMA Psychiatry. (2016) 73:150–8. doi: 10.1001/jamapsychiatry.2015.2688
4. Cunningham, R, Stanley, J, Haitana, T, Pitama, S, Crowe, M, Mulder, R, et al. The physical health of Māori with bipolar disorder. Aust N Z J Psychiatry. (2020) 54:1107–14. doi: 10.1177/0004867420954290
5. Firth, J, Siddiqi, N, Koyanagi, A, Siskind, D, Rosenbaum, S, Galletly, C, et al. The lancet psychiatry commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. (2019) 6:675–712. doi: 10.1016/S2215-0366(19)30132-4
6. Druss, BG, and von Esenwein, SA. Improving general medical care for persons with mental and addictive disorders: systematic review. Gen Hosp Psychiatry. (2006) 28:145–53. doi: 10.1016/j.genhosppsych.2005.10.006
7. Cabassa, LJ, Gomes, AP, Meyreles, Q, Capitelli, L, Younge, R, Dragatsi, D, et al. Primary health care experiences of Hispanics with serious mental illness: a mixed-methods study. Adm Policy Ment Health Ment Health Serv Res. (2014) 41:724–36. doi: 10.1007/s10488-013-0524-2
8. Happell, B, Ewart, SB, Bocking, J, Platania-Phung, C, and Stanton, R. ‘That red flag on your file’: misinterpreting physical symptoms as mental illness. J Clin Nurs. (2016) 25:2933–42. doi: 10.1111/jocn.13355
9. Clarke, DE, Dusome, D, and Hughes, L. Emergency department from the mental health client’s perspective. Int J Ment Health Nurs. (2007) 16:126–31. doi: 10.1111/j.1447-0349.2007.00455.x
10. Shefer, G, Henderson, C, Howard, LM, Murray, J, and Thornicroft, G. Diagnostic overshadowing and other challenges involved in the diagnostic process of patients with mental illness who present in emergency departments with physical symptoms – a qualitative study. PLoS One. (2014) 9:e111682. doi: 10.1371/journal.pone.0111682
11. Jones, S, Howard, L, and Thornicroft, G. ‘Diagnostic overshadowing’: worse physical health care for people with mental illness. Acta Psychiatr Scand. (2008) 118:169–71. doi: 10.1111/j.1600-0447.2008.01211.x
12. Nash, M. Diagnostic overshadowing: a potential barrier to physical health care for mental health service users. Ment Health Pract. (2013) 17:22–6. doi: 10.7748/mhp2013.12.17.4.22.e862
13. Knaak, S, Mantler, E, and Szeto, A. Mental illness-related stigma in healthcare. Healthc Manage Forum. (2017) 30:111–6. doi: 10.1177/0840470416679413
14. Vistorte, AOR, Ribeiro, WS, Jaen, D, Jorge, MR, Evans-Lacko, S, and Mari, JDJ. Stigmatizing attitudes of primary care professionals towards people with mental disorders: a systematic review. Int J Psychiatry Med. (2018) 53:317–38. doi: 10.1177/0091217418778620
15. Molloy, R, Munro, I, and Pope, N. Understanding the experience of diagnostic overshadowing associated with severe mental illness from the consumer and health professional perspective: a qualitative systematic review protocol. JBI Evid Synth. (2020) 19:1362–8. doi: 10.11124/JBIES-20-00244
16. Thornicroft, G, Rose, D, Kassam, A, and Sartorius, N. Stigma: ignorance, prejudice or discrimination? Br J Psychiatry. (2007) 190:192–3. doi: 10.1192/bjp.bp.106.025791
17. Corrigan, PW, and Watson, A. Understanding the impact of stigma on people with mental illness. World Psychiatry. (2002) 1:16–20.
18. FitzGerald, C, and Hurst, S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. (2017) 18:19. doi: 10.1186/s12910-017-0179-8
19. Rössler, W. The stigma of mental disorders. EMBO Rep. (2016) 17:1250–3. doi: 10.15252/embr.201643041
20. Peterson, D, Pere, L, Sheehan, N, and Surgenor, G. Respect costs nothing: A survey of discrimination faced by people with experience of mental illness in Aotearoa New Zealand. Auckland: Mental Health Foundation of New Zealand (2004).
21. Van Nieuwenhuizen, A, Henderson, C, Kassam, A, Graham, T, Murray, J, Howard, LM, et al. Emergency department staff views and experiences on diagnostic overshadowing related to people with mental illness. Epidemiol Psychiatr Sci. (2013) 22:255–62. doi: 10.1017/S2045796012000571
22. Every-Palmer, S, Romans, SE, Stubbs, R, Tomlinson, A, Gandhi, S, and Huthwaite, M. Experiences of weight-loss surgery in people with serious mental illness: a qualitative study. Front Psych. (2020) 11:419. doi: 10.3389/fpsyt.2020.00419
23. Corrigan, PW, Druss, BG, and Perlick, DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. (2014) 15:37–70. doi: 10.1177/1529100614531398
24. Rivera-Segarra, E, Varas-Díaz, N, and Santos-Figueroa, A. “That’s all fake”: health professionals stigma and physical healthcare of people living with serious mental illness. PLoS One. (2019) 14:e0226401. doi: 10.1371/journal.pone.0226401
25. Ross, LE, Vigod, S, Wishart, J, Waese, M, Spence, JD, Oliver, J, et al. Barriers and facilitators to primary care for people with mental health and/or substance use issues: a qualitative study. BMC Fam Pract. (2015) 16:135. doi: 10.1186/s12875-015-0353-3
26. Lester, H, Tritter, JQ, and Sorohan, H. Patients' and health professionals' views on primary care for people with serious mental illness: focus group study. BMJ. (2005) 330:1122. doi: 10.1136/bmj.38440.418426.8F
27. Morgan, AJ, Reavley, NJ, Jorm, AF, and Beatson, R. Experiences of discrimination and positive treatment from health professionals: a national survey of adults with mental health problems. Aust N Z J Psychiatry. (2016) 50:754–62. doi: 10.1177/0004867416655605
28. Ewart, SB, Bocking, J, Happell, B, Platania-Phung, C, and Stanton, R. Mental health consumer experiences and strategies when seeking physical health care. Glob Qual Nurs Res. (2016) 3:233339361663167. doi: 10.1177/2333393616631679
29. Haitana, T, Pitama, S, Cormack, D, Rangimarie Clark, MT, and Lacey, C. 'It absolutely needs to move out of that structure': Māori with bipolar disorder identify structural barriers and propose solutions to reform the New Zealand mental health system. Ethn Health. (2022) 28:234–56. doi: 10.1080/13557858.2022.2027884
30. Haitana, T, Pitama, S, Cormack, D, Clark, MTR, and Lacey, C. Culturally competent, safe and equitable clinical care for Māori with bipolar disorder in New Zealand: the expert critique of Māri patients and Whānau. Aust N Z J Psychiatry. (2022) 56:648–56. doi: 10.1177/00048674211031490
31. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
32. Molloy, R, Brand, G, Munro, I, and Pope, N. Seeing the complete picture: a systematic review of mental health consumer and health professional experiences of diagnostic overshadowing. J Clin Nurs. (2021) 32:1–12. doi: 10.1111/jocn.16151
33. Corrigan, PW, Mittal, D, Reaves, CM, Haynes, TF, Han, X, Morris, S, et al. Mental health stigma and primary health care decisions. Psychiatry Res. (2014) 218:35–8. doi: 10.1016/j.psychres.2014.04.028
34. Melamed, OC, Fernando, I, Soklaridis, S, Hahn, MK, Lemessurier, KW, and Taylor, VH. Understanding engagement with a physical health service: a qualitative study of patients with severe mental illness. Can J Psychiatry. (2019) 64:872–80. doi: 10.1177/0706743719862980
35. Chew-Graham, CA, Heyland, S, Kingstone, T, Shepherd, T, Buszewicz, M, Burroughs, H, et al. Medically unexplained symptoms: continuing challenges for primary care. Br J Gen Pract. (2017) 67:106–7. doi: 10.3399/bjgp17X689473
36. Husain, M, and Chalder, T. Medically unexplained symptoms: assessment and management. Clin Med. (2021) 21:13–8. doi: 10.7861/clinmed.2020-0947
37. National Institute for Health and Care Excellence (NICE). Chronic pain (primary and secondary) in over 16s: Assessment of all chronic pain and management of chronic primary pain. (NICE guideline 193). National Institute for Health and Care Excellence. (2021). Available at https://www.nice.org.uk/guidance/ng193.
38. Bransfield, RC, and Friedman, KJ. Differentiating psychosomatic, somatopsychic, multisystem illnesses, and medical uncertainty. Healthcare (Basel). (2019) 7:114. doi: 10.3390/healthcare7040114
39. FitzGerald, C, Martin, A, Berner, D, and Hurst, S. Interventions designed to reduce implicit prejudices and implicit stereotypes in real world contexts: a systematic review. BMC Psychol. (2019) 7:29. doi: 10.1186/s40359-019-0299-7
40. Keene, L. The path to patient-centred care. Wellington: Association of Salaried Medical Specialists (2016).
41. Ungar, T, Knaak, S, and Szeto, AC. Theoretical and practical considerations for combating mental illness stigma in health care. Community Ment Health J. (2016) 52:262–71. doi: 10.1007/s10597-015-9910-4
42. Ireson, J, Taylor, A, Richardson, E, Greenfield, B, and Jones, G. Exploring invisibility and epistemic injustice in long Covid-a citizen science qualitative analysis of patient stories from an online Covid community. Health Expect. (2022) 25:1753–65. doi: 10.1111/hex.13518
43. Rees, SN, Crowe, M, and Harris, S. The lesbian, gay, bisexual and transgender communities' mental health care needs and experiences of mental health services: an integrative review of qualitative studies. J Psychiatr Ment Health Nurs. (2021) 28:578–89. doi: 10.1111/jpm.12720
44. Khan, M, Ilcisin, M, and Saxton, K. Multifactorial discrimination as a fundamental cause of mental health inequities. Int J Equity Health. (2017) 16:43. doi: 10.1186/s12939-017-0532-z
45. Das-Munshi, J, Stewart, R, Morgan, C, Nazroo, J, Thornicroft, G, and Prince, M. Reviving the ‘double jeopardy’ hypothesis: physical health inequalities, ethnicity and severe mental illness. Br J Psychiatry. (2016) 209:183–5. doi: 10.1192/bjp.bp.114.159210
46. Stepanikova, I, Acharya, S, Abdalla, S, Baker, E, Klanova, J, and Darmstadt, GL. Gender discrimination and depressive symptoms among child-bearing women: ELSPAC-CZ cohort study. EClinicalMedicine. (2020) 20:100297. doi: 10.1016/j.eclinm.2020.100297
47. Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington (DC): National Academies Press (US) (2001).
48. Håkansson Eklund, J, Holmström, IK, Kumlin, T, Kaminsky, E, Skoglund, K, Höglander, J, et al. “Same same or different?” a review of reviews of person-centered and patient-centered care. Patient Educ Couns. (2019) 102:3–11. doi: 10.1016/j.pec.2018.08.029
49. Latoo, J, Mistry, M, Alabdulla, M, Wadoo, O, Jan, F, Munshi, T, et al. Mental health stigma: the role of dualism, uncertainty, causation and treatability. Gen Psychiatr. (2021) 34:e100498. doi: 10.1136/gpsych-2021-100498
50. Fitzgerald, M. Do psychiatry and neurology need a close partnership or a merger? BJPsych Bull. (2015) 39:105–7. doi: 10.1192/pb.bp.113.046227
51. Naylor, C, Preety, D, Ross, S, and Al, E. Bringing together physical and mental health: A frontier for integrated care. London: The King's Fund and Centre for Mental Health (2016).
52. World Health Organization. Integrating mental health into primary care: A global perspective. Geneva: WHO Press, World Health Organization (2008).
53. Richardson, A, Richard, L, Gunter, K, Cunningham, R, Hamer, H, Lockett, H, et al. A systematic scoping review of interventions to integrate physical and mental healthcare for people with serious mental illness and substance use disorders. J Psychiatr Res. (2020) 128:52–67. doi: 10.1016/j.jpsychires.2020.05.021
54. Coates, D, Coppleson, D, and Schmied, V. Integrated physical and mental healthcare: an overview of models and their evaluation findings. Int J Evid Based Healthc. (2020) 18:38–57. doi: 10.1097/XEB.0000000000000215
55. Rodgers, M, Dalton, J, Harden, M, Street, A, Parker, G, and Eastwood, A. Integrated care to address the physical health needs of people with severe mental illness: a mapping review of the recent evidence on barriers, facilitators and evaluations. International. J Integr Care. (2018) 18:9. doi: 10.5334/ijic.2605
56. Brown, M, Moore, CA, Macgregor, J, and Lucey, JR. Primary care and mental health: overview of integrated care models. J Nurse Pract. (2021) 17:10–4. doi: 10.1016/j.nurpra.2020.07.005
57. McInnes, S, Halcomb, E, Ashley, C, Kean, A, Moxham, L, and Patterson, C. An integrative review of primary health care nurses’ mental health knowledge gaps and learning needs. Collegian. (2022) 29:540–8. doi: 10.1016/j.colegn.2021.12.005
58. Leigh, H, Stewart, D, and Mallios, R. Mental health and psychiatry training in primary care residency programs. Part II. What skills and diagnoses are taught, how adequate, and what affects training directors' satisfaction? Gen Hosp Psychiatry. (2006) 28:195–204. doi: 10.1016/j.genhosppsych.2005.10.004
59. Royal College of Psychiatrists. Working Group for Improving the physical health of people with SMI. Improving the physical health of adults with severe mental illness: Essential actions (OP100). London: Royal College of Psychiatrists (2016).
60. Cunningham, R, Imlach, F, Lockett, H, Lacey, C, Haitana, T, Every-Palmer, S, et al. Do patients with mental health and substance use conditions experience discrimination and diagnostic overshadowing in primary care in Aotearoa New Zealand? Results from a national online survey. J Prim Health Care. (2023) 15:112–21. doi: 10.1071/HC23015
Keywords: discrimination, health care, mental health, quality of care, overshadowing, severe mental disorder, substance use disorder
Citation: Cunningham R, Imlach F, Haitana T, Every-Palmer S, Lacey C, Lockett H and Peterson D (2023) It’s not in my head: a qualitative analysis of experiences of discrimination in people with mental health and substance use conditions seeking physical healthcare. Front. Psychiatry. 14:1285431. doi: 10.3389/fpsyt.2023.1285431
Edited by:
Samer El Hayek, Erada Center for Treatment and Rehab, United Arab EmiratesReviewed by:
Ramzi Haddad, Lebanese University, LebanonLindsay Sheehan, Illinois Institute of Technology, United States
April Prunty, Allina Health, United States
Copyright © 2023 Cunningham, Imlach, Haitana, Every-Palmer, Lacey, Lockett and Peterson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ruth Cunningham, Ruth.cunningham@otago.ac.nz
 Ruth Cunningham
Ruth Cunningham Fiona Imlach
Fiona Imlach Tracy Haitana
Tracy Haitana Susanna Every-Palmer3
Susanna Every-Palmer3