On Sunday, Prime Minister Jacinta Ardern and health director-general Dr Ashley Bloomfield confirmed that 10 Covid-19 cases in Nelson have the Omicron variant.
The cases are members of one family. All eligible members are double vaccinated. The group recently attended a wedding and other events in Auckland. There were well over 100 people at these events. There is no clear link to the border.
The prime minister said this means Omicron is now circulating in Auckland and possibly the Nelson-Marlborough region, if not elsewhere. The cabinet has therefore decided to move the country to Traffic Light System RED with full effect from today.
Projecting the numbers
Government modelling suggests Omicron could reach 1,000 cases a day within three weeks and 7,000 cases per day within six weeks including up to 1,800 cases per day in Auckland.
Omicron is hyper-infectious and transmissible. There is a lower percentage of severe cases, hospitalisations, and deaths. However, a small percentage of extremely sick people in a very large-scale Omicron event could overwhelm the health system.
Traffic Light Red
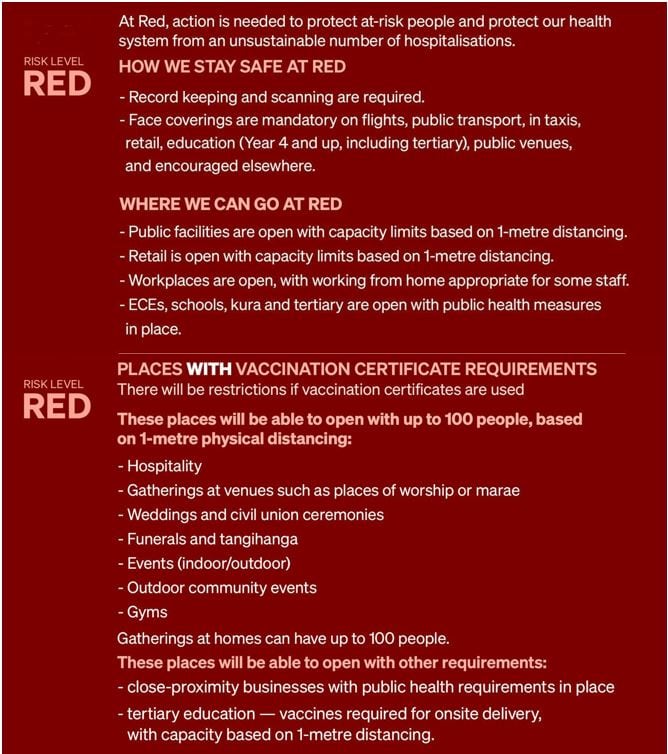
Traffic Light Red is not a lockdown:
- Businesses can continue with capacity limits based on 1-metre spacing
- Hospitality using vaccine passes can have up to 100 people seated and single servers. Hospitality venues without vaccine passes must be contactless.
- Masks and social distancing are important in retail outlets, public transport, public venues, schools, education, and health facilities. Schools can remain open with masks required at year four and above.
- Events with vaccine passes can have to 100 people attend. Events without vaccine passes are limited to 25.
- There are also different requirements for places using or not using vaccine passes.

Health and demographics risks for Māori
Māori and Pacific communities, the unvaccinated, the poor and the disabled are those most at risk from Omicron.
Māori have an elevated risk of infection because of higher comorbidities, including cancer, high blood pressure, heart disease, respiratory illnesses like asthma, diabetes, obesity, liver or kidney disease, inflammatory conditions, immunodeficient states and autoimmune diseases.
Māori also face risk because of lower access to health services. Many Māori in areas such as Te Tai Rāwhiti, Northland, the West Coast and the Bay of Plenty live some distance from emergency health care. Healthcare in many larger Māori population semi-rural areas lacks adequate intensive care capacity.
The overall socio-economic and demographic Māori profile creates a specific higher transmissibility risk that Omicron can easily exploit. For instance, more Māori live in overcrowded or temporary housing. Our population is younger and more social. More Māori are in prison. Māori have higher rates of mental illness. Each is a vector for higher transmission. A greater percentage of Māori are contract or casual workers.
Vaccination rollout vulnerabilities
Last year’s age-based vaccination rollout disadvantaged Māori because it pushed our vulnerable but more youthful population to the back of the vaccination queue.
Māori and other health providers have made a magnificent effort closing this gap from 23.2 per cent in mid-September to 10.3 per cent. However, this still leaves 17.6 per cent of Māori aged over 12 years unvaccinated and therefore particularly vulnerable to the hyper-infectious Omicron variant.
Booster shot inequity
The international evidence has shown the effectiveness of double vaccination decreases faster against Omicron than the Delta variant. A third booster Pfizer dose increases protection:
- 55 to 65 percent effective against infection.
- 70 percent protection from symptomatic illness.
- 90 percent protection against hospitalisation including in older populations over 65 years.
New Zealand began the third booster rollout on January 5, with a qualifying period of four months after the second vaccination.
On Sunday’s numbers, the Māori uptake of boosters at 18.9 per cent of the eligible over-18 years population is also well behind the national average of 27.0 per cent.
The 105,00 Māori vaccinated since November 1 will also not qualify for the booster shot until March 1 or later. This is too late to avoid a substantial risk of Omicron devastating Māori communities.
The government must shorten the qualifying period to three months to meet its obligation under Te Tiriti o Waitangi to actively protect the lives of Māori. Britain allows boosters after three months for vulnerable communities. Australia has also changed to a three-month waiting period.
Tamariki Māori vaccination
Preliminary data from early last week shows the tamariki Māori 5 to 11 years rollout in Auckland is running at 50% of those for non-Māori/Pacific children.
The government and ministry must appoint a tamariki vaccination monitoring group with access to data and be able to discuss the rollout with officials and the government and do so now.
Preparing for Omicron
Omicron will place significant pressure on the health system. Many Māori homes and communities will be left to care for themselves. There will also be supply interruptions with higher numbers of workers sick and isolating at home.
The following is a basic essential 10-point list to protect whānau and whakapapa during higher case numbers in an Omicron outbreak.
1. Develop a plan for isolating infected members of your whānau separate from others at home.
2. Face coverings, gloves, hand sanitiser or other disinfectant, tissues or old towels, rubbish bags and basic budget surface cleaning supplies will be important items for protecting your whanau. Do not hesitate to think budget. Most off-the-shelf ready-to-use general kitchen, laundry and bathroom surface cleaners are multi-purpose.
3. If possible, try to have enough food for the household for up to seven days.
4. Many whānau will be unable to afford such a reserve. In that instance, it is important to connect and let other whānau, Māori or mainstream community initiatives like food banks know your situation so they can provide support.
5. Gather things together that we use when we have a bad head cold flu, like paracetamol, ibuprofen, throat lozenges, ice blocks, drinks, cup of soup sachets and vapour rubs. This will be challenging for many whānau. Budget brands from supermarkets or online are often the same and much cheaper than more expensive brands. These will not cure Covid-19 but they will help manage symptoms.
6. If you are isolating at home find someone outside your household who would be able to help with delivering food, medicines, or other essential items.
7. If the house has more than one bathroom, one should be allocated to Covid-positive people. In households with a single bathroom, clean surfaces after every use, leave windows open and fans on.
8. Do not hesitate to reach out for help or advice from mainstream or Māori health providers, Ministry of Health online services or other community groups. Māori providers will understand your situation best. Your welfare is important.
9. Do not neglect your mental health. Books, games, craft or DIY activities, access to the internet and streaming services can all help keep boredom at bay.
10. If comfortable, hang a sign or Covid-19 Tracer QR Code on your door advising visitors that you are isolating.
Kia kaha koutou kia noho haumaru tō whānau. Stay safe.
Dr Rawiri Taonui