Abstract
Purpose
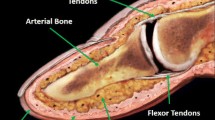
Bio-impedance analysis (BIA) has been widely investigated for hemodynamic monitoring. However, previous works rarely modelled two synchronously pulsatile arteries (representing the radial and ulnar arteries) in the wrist/forearm model. This work aims to clarify and quantify the influences of two pulsatile arteries on BIA.
Methods
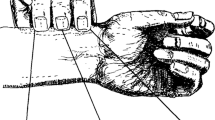
First, two blood-filled arteries were structured in a 3D wrist segment using the finite element method (FEM). Afterwards, an easy-to-produce two-arteries artificial wrist was fabricated with two components: gelatine-based surrounding tissue phantom and saline blood phantom. A syringe driver was utilised to constrict the arteries, and the impedance signals were measured using a Multi-frequency Impedance Analyser (MFIA).
Results
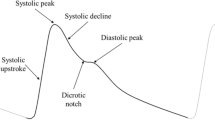
Both simulation and experimental results demonstrated the non-negligible influences of the ulnar artery on the overall BIA, inducing unwanted resistance changes to the acquired signals from the radial artery. The phantom experiments revealed the summation of the individual resistance changes caused by a single pulsatile artery was approximately equal to the measured resistance change caused by two synchronously pulsatile arteries, confirming the measured impedance signal at the wrist contains the pulsatile information from both arteries.
Conclusion
This work is the first simulation and phantom investigation into two synchronously pulsatile arteries under BIA in the distal forearm, providing a better insight and understanding in the morphology of measured impedance signals. Future research can accordingly select either a small spacing 4-spot electrode configuration for a single artery sensing or a band electrode configuration for overall pulsatile arteries sensing. A more accurate estimation of blood volume change and pulse wave analysis (PWA) could help to develop cuffless blood pressure measurement (BPM).











Similar content being viewed by others
References
Ramsingh, D., B. Alexander, and M. Cannesson. Clinical review: does it matter which hemodynamic monitoring system is used? Crit. Care. 17(2):208, 2012. https://doi.org/10.1186/cc11814.
Truijen, J., J. J. van Lieshout, W. A. Wesselink, and B. E. Westerhof. Noninvasive continuous hemodynamic monitoring. J. Clin. Monit. Comput. 26(4):267–278, 2012. https://doi.org/10.1007/s10877-012-9375-8.
Scheeren, T. W. L., and M. A. E. Ramsay. New developments in hemodynamic monitoring. J. Cardiothorac. Vasc. Anesth. 33:S67–S72, 2019. https://doi.org/10.1053/j.jvca.2019.03.043.
MateuCampos, M. L., et al. Techniques available for hemodynamic monitoring. Advantages and limitations. Med. Intensiva (Engl. Ed.). 36(6):434–444, 2012. https://doi.org/10.1016/j.medine.2012.09.004.
Pinsky, M. R., and D. Payen. Functional hemodynamic monitoring. Crit. Care. 9(6):566, 2005. https://doi.org/10.1186/cc3927.
Briesenick, L., F. Michard, and B. Saugel. Mobile devices for hemodynamic monitoring. In: Annual Update in Intensive Care and Emergency Medicine, edited by J.-L. Vincent. Cham: Springer International Publishing, 2020, pp. 655–665. https://doi.org/10.1007/978-3-030-37323-8_50.
Biswas, D., N. Simoes-Capela, C. Van Hoof, and N. Van Helleputte. Heart rate estimation from wrist-worn photoplethysmography: a review. IEEE Sens. J. 19(16):6560–6570, 2019. https://doi.org/10.1109/JSEN.2019.2914166.
Jung, M. H., et al. Wrist-wearable bioelectrical impedance analyzer with miniature electrodes for daily obesity management. Sci. Rep. 11(1):1238, 2021. https://doi.org/10.1038/s41598-020-79667-3.
Anand, G., Y. Yu, A. Lowe, and A. Kalra. Bioimpedance analysis as a tool for hemodynamic monitoring: overview, methods and challenges. Physiol. Meas. 42(3):03TR01, 2021. https://doi.org/10.1088/1361-6579/abe80e.
Alharbi, Y., A. Alshrouf, and S. Mansouri. Heart rate monitoring using electrical impedance. In: 2021 Seventh International Conference on Bio Signals, Images, and Instrumentation (ICBSII). Chennai: IEEE, 2021, pp. 1–4. https://doi.org/10.1109/ICBSII51839.2021.9445147.
De Pinho Ferreira, N., C. Gehin, and B. Massot. A review of methods for non-invasive heart rate measurement on wrist. IRBM. 42(1):4–18, 2021. https://doi.org/10.1016/j.irbm.2020.04.001.
Lee, W., and S. Cho. Integrated all electrical pulse wave velocity and respiration sensors using bio-impedance. IEEE J. Solid-State Circuits. 50(3):776–785, 2015. https://doi.org/10.1109/JSSC.2014.2380781.
Sel, K., A. Brown, H. Jang, H. M. Krumholz, N. Lu, and R. Jafari. A wrist-worn respiration monitoring device using bio-impedance. In: 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC). Montreal, QC: IEEE, 2020, pp. 3989–3993. https://doi.org/10.1109/EMBC44109.2020.9176367.
Bang, S., C. Lee, J. Park, M.-C. Cho, Y.-G. Yoon, and S. Cho. A pulse transit time measurement method based on electrocardiography and bioimpedance. In: 2009 IEEE Biomedical Circuits and Systems Conference. Beijing: IEEE, 2009, pp. 153–156. https://doi.org/10.1109/BIOCAS.2009.5372060.
Huynh, T., R. Jafari, and W.-Y. Chung. An accurate bioimpedance measurement system for blood pressure monitoring. Sensors. 18(7):2095, 2018. https://doi.org/10.3390/s18072095.
Dujardin, J. P., D. N. Stone, C. D. Forcino, L. T. Paul, and H. P. Pieper. Effects of blood volume changes on characteristic impedance of the pulmonary artery. Am. J. Physiol. Heart Circ. Physiol. 242(2):H197–H202, 1982. https://doi.org/10.1152/ajpheart.1982.242.2.H197.
Liebman, F. M., and S. Bagno. The behavior of the red blood cells in flowing blood which accounts for conductivity changes. Biomed. Sci. Instrum. 4:25–35, 1968.
Cho, M.-C., J.-Y. Kim, and S. Cho. A bio-impedance measurement system for portable monitoring of heart rate and pulse wave velocity using small body area. In: 2009 IEEE International Symposium on Circuits and Systems. Taipei: IEEE, 2009, pp. 3106–3109. https://doi.org/10.1109/ISCAS.2009.5118460.
Bradley, C. K., et al. Cuffless blood pressure devices. Am. J. Hypertens. 2022. https://doi.org/10.1093/ajh/hpac017.
Romero-Beltrán, C. A., A. M. González-Vargas, and J. J. Cabrera-López. Non-invasive blood pressure as an application of electrical impedance: a short review. J. Phys.: Conf. Ser. 2008(1):012013, 2021. https://doi.org/10.1088/1742-6596/2008/1/012013.
Liu, S.-H., D.-C. Cheng, and C.-H. Su. A cuffless blood pressure measurement based on the impedance plethysmography technique. Sensors. 17(5):1176, 2017. https://doi.org/10.3390/s17051176.
Huynh, T. H., R. Jafari, and W.-Y. Chung. Noninvasive cuffless blood pressure estimation using pulse transit time and impedance plethysmography. IEEE Trans. Biomed. Eng. 2018. https://doi.org/10.1109/TBME.2018.2865751.
Mukkamala, R., G. S. Stergiou, and A. P. Avolio. Cuffless blood pressure measurement. Annu. Rev. Biomed. Eng. 24(1):203–230, 2022. https://doi.org/10.1146/annurev-bioeng-110220-014644.
Lin, W.-H., F. Chen, Y. Geng, N. Ji, P. Fang, and G. Li. Towards accurate estimation of cuffless and continuous blood pressure using multi-order derivative and multivariate photoplethysmogram features. Biomed. Signal Process. Control 63:102198, 2021. https://doi.org/10.1016/j.bspc.2020.102198.
El-Hajj, C., and P. A. Kyriacou. Cuffless blood pressure estimation from PPG signals and its derivatives using deep learning models. Biomed. Signal Process. Control.70:102984, 2021. https://doi.org/10.1016/j.bspc.2021.102984.
Khalid, S. G., H. Liu, T. Zia, J. Zhang, F. Chen, and D. Zheng. Cuffless blood pressure estimation using single channel photoplethysmography: a two-step method. IEEE Access. 8:58146–58154, 2020. https://doi.org/10.1109/ACCESS.2020.2981903.
Ibrahim, B., and R. Jafari. Cuffless blood pressure monitoring from a wristband with calibration-free algorithms for sensing location based on bio-impedance sensor array and autoencoder. Sci. Rep. 12(1):319, 2022. https://doi.org/10.1038/s41598-021-03612-1.
Sugawara, M., K. Niki, H. Furuhata, S. Ohnishi, and S. Suzuki. Relationship between the pressure and diameter of the carotid artery in humans. Heart Vessels. 15(1):49–51, 2000. https://doi.org/10.1007/PL00007261.
Metshein, M., P. Annus, R. Land, M. Min, and A. Aabloo. Availability and variations of cardiac activity in the case of measuring the bioimpedance of wrist. In: 2018 IEEE International Instrumentation and Measurement Technology Conference (I2MTC). Houston, TX: IEEE, 2018, pp. 1–5. https://doi.org/10.1109/I2MTC.2018.8409684.
Pesti, K., M. Metshein, P. Annus, H. Koiv, and M. Min. Electrode placement strategies for the measurement of radial artery bioimpedance: simulations and experiments. IEEE Trans. Instrum. Meas. 70:1–10, 2021. https://doi.org/10.1109/TIM.2020.3011784.
Sel, K., N. Huerta, M. S. Sacks, and R. Jafari. Parametric modeling of human wrist for bioimpedance-based physiological sensing. In: ICASSP 2022—2022 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP). Singapore: IEEE, 2022, pp. 1161–1165. https://doi.org/10.1109/ICASSP43922.2022.9747695.
Yu, Y., G. Anand, A. Lowe, H. Zhang, and A. Kalra. Towards estimating arterial diameter using bioimpedance spectroscopy: a computational simulation and tissue phantom analysis. Sensors. 22(13):4736, 2022. https://doi.org/10.3390/s22134736.
Grampp, S., S. Majumdar, M. Jergas, P. Lang, A. Gies, and H. K. Genant. MRI of bone marrow in the distal radius: in vivo precision of effective transverse relaxation times. Eur. Radiol. 1995. https://doi.org/10.1007/BF00178080.
Karki, B. B., M. D. Bhattarai, M. R. Bajracharya, S. Karki, and A. R. Devkota. Correlation of neck and wrist circumference with waist circumference. J. Adv. Intern. Med. 3(2):47–51, 2015. https://doi.org/10.3126/jaim.v3i2.14063.
Maughan, R. J., J. S. Watson, and J. Weir. The relative proportions of fat, muscle and bone in the normal human forearm as determined by computed tomography. Clin. Sci. 66(6):683–689, 1984. https://doi.org/10.1042/cs0660683.
Toomayan, G. A., F. Robertson, N. M. Major, and B. E. Brigman. Upper extremity compartmental anatomy: clinical relevance to radiologists. Skelet. Radiol. 35(4):195–201, 2006. https://doi.org/10.1007/s00256-005-0063-3.
Weinberg, L., M. Spanger, C. Tan, and M. Nikfarjam. Postoperative wristwatch-induced compressive neuropathy of the hand: a case report. J Med. Case Rep. 9(1):141, 2015. https://doi.org/10.1186/s13256-015-0625-5.
Ashraf, T., Z. Panhwar, S. Habib, M. A. Memon, F. Shamsi, and J. Arif. Size of radial and ulnar artery in local population. J. Pak. Med. Assoc. 60(10):817–819, 2010.
Beniwal, S., K. Bhargava, and S. K. Kausik. Size of distal radial and distal ulnar arteries in adults of southern Rajasthan and their implications for percutaneous coronary interventions. Indian Heart J. 66(5):506–509, 2014. https://doi.org/10.1016/j.ihj.2014.08.010.
Riekkinen, H. V., K. O. Karkola, and A. Kankainen. The radial artery is larger than the ulnar. Ann. Thorac. Surg. 75(3):882–884, 2003. https://doi.org/10.1016/S0003-4975(02)04557-5.
Gabriel, C., S. Gabriel, and E. Corthout. The dielectric properties of biological tissues: I. Literature survey. Phys. Med. Biol. 41(11):2231–2249, 1996. https://doi.org/10.1088/0031-9155/41/11/001.
Gabriel, S., R. W. Lau, and C. Gabriel. The dielectric properties of biological tissues: II. Measurements in the frequency range 10 Hz to 20 GHz. Phys. Med. Biol. 41(11):2251–2269, 1996. https://doi.org/10.1088/0031-9155/41/11/002.
Gabriel, S., R. W. Lau, and C. Gabriel. The dielectric properties of biological tissues: III. Parametric models for the dielectric spectrum of tissues. Phys. Med. Biol. 41(11):2271–2293, 1996. https://doi.org/10.1088/0031-9155/41/11/003.
‘IEC 60601’, Wikipedia. June 10, 2022. Available https://en.wikipedia.org/w/index.php?title=IEC_60601&oldid=1092467861. Accessed 16 June 2022.
Yu, Y., A. Lowe, G. Anand, and A. Kalra. Tissue phantom to mimic the dielectric properties of human muscle within 20 Hz and 100 kHz for biopotential sensing applications. In: 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). Berlin: IEEE, 2019, pp. 6490–6493. https://doi.org/10.1109/EMBC.2019.8856530.
Anand, G., A. Lowe, and A. M. Al-Jumaily. Simulation of impedance measurements at human forearm within 1 kHz to 2 MHz. J. Electr. Bioimpedance. 7(1):20, 2016. https://doi.org/10.5617/jeb.2657.
Mohamed, R., M. El Dosoky, and M. El-Wakad. The effect of heart pulsatile on the measurement of artery bioimpedance. J. Electr. Bioimpedance. 8(1):101, 2017. https://doi.org/10.5617/jeb.4677.
Shash, Y. H., M. A. A. Eldosoky, and M. T. Elwakad. Detection of stenosis in blood vessel by using bio-impedance analysis. In: 2018 35th National Radio Science Conference (NRSC). Cairo: IEEE, 2018, pp. 503–512. https://doi.org/10.1109/NRSC.2018.8354409.
Huang, J.-J., Y.-M. Huang, and A. R. See. Studying peripheral vascular pulse wave velocity using bio-impedance plethysmography and regression analysis. ECTI Trans. Comput. Inf. Technol. 11(1):63–70, 2017. https://doi.org/10.37936/ecti-cit.2017111.64861.
Kim, H., E. Kim, C. Choi, and W.-H. Yeo. Advances in soft and dry electrodes for wearable health monitoring devices. Micromachines. 13(4):629, 2022. https://doi.org/10.3390/mi13040629.
Zhang, H., A. Kalra, A. Lowe, Y. Yu, and G. Anand. A hydrogel-based electronic skin for touch detection using electrical impedance tomography. Sensors. 23(3):1571, 2023. https://doi.org/10.3390/s23031571.
Acknowledgements
This study was conducted at the Institute of Biotechnology (IBtec) as part of the PhD Program funded by the School of Engineering, Computer and Mathematical Sciences, Auckland University of Technology.
Funding
This research was funded by Institute of Biomedical Technologies (IBTec), the School of Engineering, Computer and Mathematical Sciences, Auckland University of Technology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Associate Editor Derek J. Dosdall oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, Y., Lowe, A., Anand, G. et al. The Investigation of Bio-impedance Analysis at a Wrist Phantom with Two Pulsatile Arteries. Cardiovasc Eng Tech 14, 810–826 (2023). https://doi.org/10.1007/s13239-023-00689-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-023-00689-9